This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
CASE
A 65 year old man, mason by occupation came to the casuality with
CHIEF COMPLAINTS :
Weakness of left upper and lower limb since 1 month
HISTORY OF PRESENT ILLNESS :
Patient was apparently asymptomatic 1 month back then he developed weakness of Left upper and lower limbs
His earliest recall of events dates back to
26/12/2020 :
Where,on this day he woke up early in the morning at 6am and got up from his bed and started walking towards the washroom, he relieved himself and then came back doing his routine work like every day. As his wife called him for breakfast and when he was having it, suddenly he felt weakness in the left upper limbs and as he was trying to hold the glass of water for few sips ,and after as he was trying to stand ,he couldnt feel the ground with his left leg.The couple immediately called their son who hurried to the scene. Sensing the problem, his son took him to our hospital. He had intake of alcohol 180 ml whisky the previous night prior to this presentation. He stayed in hospital for about 1 week and treated conservatively (tab ecospirin 75mg, clopitab 75mg and atorvastatin 20mg for 2 weeks) and was adviced to have physiotherapy of Left Upper and lower limb at home. After 2 weeks of discharge his weakness was resolved and he continued his daily routine work after that.
I redirect the conversation to the current incident and the patient reports that his weakness started again since 1 month, which was gradually progressed over a few days from onset(espically left lower limb).On probing further he says, he has the most
difficulty in getting up from a squatting position, standing up from a chair without support, and while walking he has to stress his other normal lower limb to walk, that to with great difficulty. He also complains of stiffness and dragging type of pain in his left lower limb.
He recalls being delinquent at the age of 20 years, when he started smoking beedis 1 pack per day regularly and consumed cheap liquor (whisky) 90-180ml regularly. He says they relax him after a hard day's work. He furthur says that he quitted consuming alcohol 1 year back and smoking 3 years back.
He was diagnosed to be hypertensive since 2 years on routine check up at his village and on regular medication (tab Amlong 5 mg + tab Atenolol 50 mg OD). From 9 months he was using tab Telma 40 mg/OD
The patient is able to respond well to my questions, with appropriate responses. He denies having loss of smell, double vision or loss of sight. He denies having unusual sensations on his face and a difficulty in chewing food. He denies history of drooping of eyelids or drooling of saliva. He also denied deviation of angle of mouth. So do the attendants. No history of change in the timbre of his voice, he denied hoarseness, nasal regurgitation of food and water or a nasal twang to his speech. He is able to swallow well.
PAST HISTORY :
He was K/C/O HTN since 2 years and was on regular medication (tab Amlong 5 mg + tab Atenolol 50 mg OD).From 9 months he was using tab Telma 40 mg/OD
Not a K/C/O Dm, CAD,TB, Asthama, Thyroid and epilepsy
No past surgical.history
No previous blood transfusions
PERSONAL HISTORY :
Mixed diet
Sleep adequate
Appetite normal
Bowel and bladder movements regular
He was a known alcoholic since 40 years.Drinks regularly 90-180 ml whisky.Quitted drinking 1 year back
Smokes 1 pack of beedi/day since 40 years.Quitted smoking 3 years back
VITALS :
GCS : E4V5M6
Temp: Afebrile
PR: 64 bpm
BP: 130/80 mm hg
RR: 15 cpm
Spo2 - 98% at RA
GRBS - 115 mg/dl
GENERAL EXAMINATION :
Patient is conscious, coherent and cooperative
Moderately built and moderately nourished
No pallor, icterus,clubbing,cyanosis, koilonychia, edema and lymphadenopathy
SYSTEMIC EXAMINATION
CVS :
Inspection:
Chest wall is bilaterally symmetrical.
No precordial bulge
Palpation:
JVP - normal
Apex beat - felt in the left 5th intercostal space in the mid clavicular line.
Auscultation:
S1, S2 heard , No murmurs
RS :
Position of trachea: central
Bilateral air entry +
NVBS heard
PER ABDOMEN :
Soft, non distended and non tender
No organomegaly
Bowel sounds heard
No palpable mass or fluid present
CNS :
Patient is Conscious
1. Higher mental functions
a) Appearance & behaviour - moderately built , oriented to time,place and person
b) Level of consciousness - conscious
c) Speech & language - Responsive
c) Cognitive functions - oriented to
time,place and person
- Memory-immediate,recent and remote memory present
- Appearence-well kept
2. Cranial nerves
1. Olfactory : Smell present on both sides
2. Optic : visual acuity - 6/6,Visual field,colour vision, reflexes : normal
3. Occulomotor, trochlear & abducent :
Pupils are reactive and normal
No ptosis & nystagmus
4. Trigeminal :
Sensory - normal on both sides
Motor - normal on both sides
Corneal reflex - present
Conjuctival reflex - present
7. Facial nerve :
Motor:
- Nasolabial folds present on both sides, no deviation of angle of mouth
- Able to close eyes
- Frowning present on both sides of forehead
- Blowing and whistling present
- Taste sensation on anterior 2/3rd of tongue present
Sensory: secretomotor moistness of eye and tongue normal, buccal mucosa normal
8. Vestibulocochlear
- Rinnes : positive
- Weber : heard qually in both ears
- Schwabach test : normal
9. Glossopharyngeal & Vagus : Gag reflex present , uvula was centrally placed
11. Spinal accessory :
Trapezieus - shrugging of shoulders present
Sternocleidomastoid - turning of head against resistance present
12. Hypoglossal : no deviation of tongue, no wasting, no fibrillations
3.Motor system :
- Attitude & position : patient in supine position
- Bulk : normal , no wasting
- TONE:
Rt Lt
UL N N
LL N hypotonia
- POWER:
Rt Lt
UL 5/5 4/5
LL 5/5 3/5
- REFLEXES :
•Superficial Rt Lt
Corneal : +2 +2
Conjunctival : +2 +2
Abdominal : +2 +2
• Deep Rt Lt
Biceps : +2 +2
Triceps : + +
Supinator : + +
Knee jerk : +2 +2
Ankle jerk : + +
Plantar : flexor flexor
4. Sensory system -
Superficial -fine touch,temperature,pain -present over all the four limbs
Deep-position ,vibration,crude touch, stereognosis, 2 point discrimination - present
Sensations decreased on left lower limb compared to right limbs
5. Cerebellum
Titubation - absent
Nystagmus- absent
Intentional tremors - absent
Pendular knee jerk - absent
Coordination tests :
Finger nose test , finger finger test ,knee heel test - coordination present
Romberg test - not elicited
Gait - Hemiparetic gait
6. No meningeal signs
FEVER CHARTING
PROVISIONAL DIAGNOSIS:
? PERIPHERAL NEUROPATHY
K/C/O LEFT HEMIPARESIS
K/c/o HTN since 2 years
Chronic alcoholic and smoker since 30 years
INVESTIGATIONS:
9/09/21
CBP
Hb - 13.3gm/dl
Tc - 10,000 cells/cumm
Neutrophils - 70%
lymphocytes - 20%
Eosinophils - 2%
Monocytes - 8%
PLT - 3.99 lakhs/cumm
CUE
Albumin - nil
Sugar - nil
Pus cells - 2-3
E.C - 2-3
RBC - nil
Casts - nil
RFT :
Serum creatinine: 0.8 mg/dl
Urea - 22 mg/dl
Sodium - 138 meq/l
K+ - 3.7 meq/l
Cl- 94 meq/l
LFT :
Total bilirubin: 0.70 mg/dl
Direct bilirubin: 0.20 mg/dl
AST: 14 IU/l
ALT: 19 IU/l
ALP: 108 IU/l
Total protein: 7.2 gm/dl
Albumin: 4.3 gm/dl
A/G: 1.48
Urinary electrolytes:
Na - 302
K - 33.6
Cl - 442
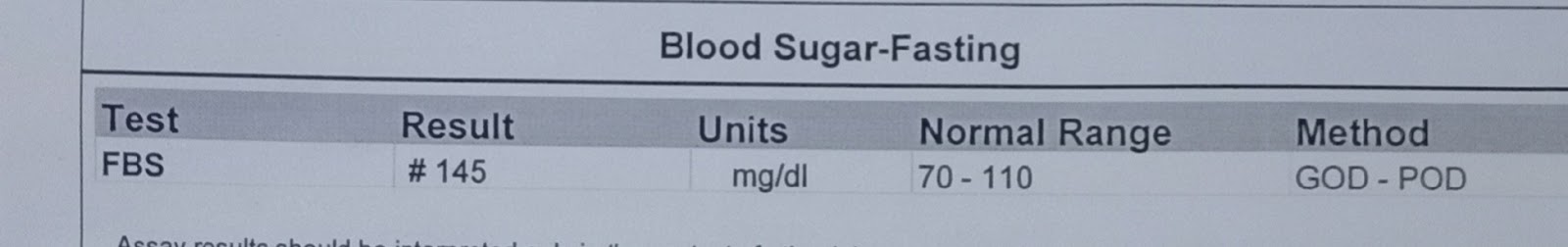
FBS
Fbs - 145 mg/dl
CXR-PA VIEW
ECG
TREATMENT :
DAY 0
1. Inj OPTINEURON 1 amp in 100 ml NS slowly UV/OD
2. Tab ECOSPIRIN - AV 75mg/20mg PO/OD
3. Tab TELMA 40mg PO/OD
4. Syp LACTULOSE 5 ml PO/TID
5. Physiotherapy of Left UL & LL
DAY 1
SOAP NOTES
SUBJECTIVE
Weakness of Left UL & LL
Dragging pain left lower limb
OBJECTIVE :
Temperature - Afebrile
BP - 90/70 mm hg
PR - 66 bpm
RR - 16 cpm
SPO2 - 98% at RA
GRBS - 115 mg/dl
ASSESSMENT
K/C/O LEFT HEMIPARESIS
K/c/o HTN since 2 years
? Peripheral neuropathy
Chronic alcoholic and smoker since 30 years
PLAN OF CARE:
1. Inj OPTINEURON 1 amp in 100 ml NS slowly IV/BD
2. Tab ECOSPIRIN - AV 75mg/20 mg PO/OD
3. Tab TELMA 40mg PO/OD
4. Tab PREGALIN -M 75 mg/po/Hs
5. Syp LACTULOSE 5 ml PO/TID
6. Physiotherapy of Left UL & LL
DAY 2
SOAP NOTES
SUBJECTIVE
Weakness of Left UL & LL
Dragging pain in left lower limb
New complaint:
Low back ache radiating to back of left thigh
OBJECTIVE :
Temperature - Afebrile
BP - 100/80 mm hg
PR - 80 bpm
RR - 16 cpm
SPO2 - 98% at RA
ASSESSMENT
? Peripheral neuropathy
K/C/O LEFT HEMIPARESIS
K/c/o HTN since 2 years
Chronic alcoholic and smoker since 30 years
PLAN OF CARE:
1. Inj OPTINEURON 1 amp in 100 ml NS slowly IV/BD
2. Tab ECOSPIRIN - AV 75mg/20 mg PO/OD
3. Tab TELMA 40mg PO/OD
4. Tab PREGABA -M 75 mg PO/HS
5. Physiotherapy of Left UL & LL
DAY 3
SOAP NOTES
SUBJECTIVE
Weakness of Left UL & LL
Dragging pain in left lower limb
Low back ache radiating to back of left thigh
OBJECTIVE :
Temperature - Afebrile
BP - 100/70 mm hg
PR - 66 bpm
RR - 15 cpm
SPO2 - 98% at RA
ASSESSMENT
? Peripheral neuropathy
K/C/O LEFT HEMIPARESIS
K/c/o HTN since 2 years
Chronic alcoholic and smoker since 30 years
PLAN OF CARE:
1. Inj OPTINEURON 1 amp in 100 ml NS slowly IV/BD
2. Tab ECOSPIRIN - AV 75mg/20 mg PO/OD
3. Tab TELMA 40mg PO/OD
4. Tab PREGABA -M 75 mg PO/HS
5. Physiotherapy of Left UL & LL
DAY 4
SOAP NOTES
SUBJECTIVE
Weakness of Left UL & LL
Dragging pain in left lower limb
Low back ache radiating to back of left thigh
OBJECTIVE :
Temperature - Afebrile
BP - 110/80 mm hg
PR - 62 bpm
RR - 15 cpm
SPO2 - 98% at RA
ASSESSMENT
? Peripheral neuropathy
K/C/O LEFT HEMIPARESIS
K/c/o HTN since 2 years
Chronic alcoholic and smoker since 30 years
PLAN OF CARE:
1. Inj OPTINEURON 1 amp in 100 ml NS slowly IV/BD
2. Tab ECOSPIRIN - AV 75mg/20 mg PO/OD
3. Tab TELMA 40mg PO/OD
4. Tab TRIGABANTIN 300 mg PO/HS
5. Tab MYORIL 4 mg PO/BD
6. Tab ULTRACET 1/2 tab QID
7. Physiotherapy of Left UL & LL
DAY 5
SOAP NOTES
SUBJECTIVE
Weakness of Left UL & LL
Dragging pain in left lower limb (decreased)
Low back ache (decreased)
OBJECTIVE :
Temperature - Afebrile
BP - 100/80 mm hg
PR - 60 bpm
RR - 15 cpm
SPO2 - 98% at RA
ASSESSMENT
? Peripheral neuropathy
K/C/O LEFT HEMIPARESIS
K/c/o HTN since 2 years
Chronic alcoholic and smoker since 30 years
PLAN OF CARE:
1. Inj OPTINEURON 1 amp in 100 ml NS slowly IV/BD
2. Tab ECOSPIRIN - AV 75mg/20 mg PO/OD
3. Tab TELMA 40mg PO/OD
4. Tab TRIGABANTIN 100 mg PO/HS
5. Tab MYORIL 4 mg PO/BD
6. Tab ULTRACET 1/2 tab QID
7. Physiotherapy of Left UL & LL















Comments
Post a Comment